In India, approximately 15-20 million couples face the challenge of infertility, accounting for nearly 25% of the global infertility burden. With the country’s fertility rate showing a dramatic decline from 6.18 in 1950 to 1.91 in 2021, more couples are turning to assisted reproductive technologies like In Vitro Fertilization (IVF). The ivf india market is growing rapidly, with a projected value of USD 1.82 billion by 2030, expanding at a CAGR of 7.8%.
This growth reflects both the increasing acceptance of fertility treatments and the rising need for such interventions among Indian couples. For many couples embarking on this journey, understanding the ivf process step by step can help reduce anxiety and create realistic expectations. This comprehensive guide focuses specifically on ivf injections, a crucial component of the treatment that often causes the most concern for patients.
Understanding Different IVF Injections and Their Purposes
Each ivf injection serves a specific purpose in the fertility treatment protocol. These medications help control your reproductive hormones and optimize the chances of successful egg retrieval, fertilization, and implantation. Familiarizing yourself with ivf injections names can help you better understand your treatment plan.
IVF Injections for Pregnancy: What Each One Does
The sequence of ivf injections for pregnancy is carefully designed to optimize your chances of success. Here’s a breakdown of the main types:

1. GnRH Agonists and Antagonists
The main purpose of these medications is to prevent premature ovulation by suppressing the body’s natural hormone cycle. The most commonly prescribed options include GnRH agonists such as Lupron, Buserelin, and Synarel, as well as GnRH antagonists like Cetrotide and Ganirelix. These medications are typically given through subcutaneous injections (under the skin), and their timing of administration differs depending on the type. GnRH agonists are usually started early in the menstrual cycle, while antagonists are introduced later during the stimulation phase.
While highly effective, these medications may come with side effects. Some of the most common include hot flashes, headaches, mood swings, and vaginal dryness. These symptoms are linked to the temporary suppression of natural hormones and generally resolve once treatment is completed. Despite these possible discomforts, their use plays a critical role in carefully controlling ovulation and improving outcomes in fertility treatments.
2. Follicle Stimulating Hormone (FSH)
The purpose of these medications is to stimulate the ovaries to produce multiple eggs, rather than the single egg that is typically released during a natural cycle. This controlled ovarian stimulation is essential in fertility treatments, as it increases the number of eggs available for retrieval and fertilisation, thereby improving the chances of success. Commonly used medications for this purpose include Gonal-F, Bravelle, and Follistim, which are designed to encourage the growth of multiple follicles in the ovaries. These are generally administered as subcutaneous injections.
They are used daily during the stimulation phase, which usually lasts between 8 to 12 days, depending on individual response. While these medications are highly effective, they can also cause certain side effects, such as bloating, abdominal discomfort, mood swings, and headaches. These reactions are generally manageable and temporary, but monitoring by a fertility specialist is crucial to ensure the ovaries are responding appropriately and to minimise risks such as ovarian hyperstimulation.
3. Human Menopausal Gonadotropin (hMG)
The purpose of these medications is to provide combined hormone stimulation, containing both follicle-stimulating hormone (FSH) and luteinizing hormone (LH). This dual action helps support follicle development while also encouraging proper hormone balance during ovarian stimulation. Commonly prescribed medications in this category include Repronex and Menopur, which can be administered either as subcutaneous or intramuscular injections depending on the treatment plan.
These medications are often used in combination with FSH-only drugs to enhance ovarian response and improve the quality of egg development. While their side effects are generally similar to those of FSH medications, patients may also experience injection site reactions such as redness, swelling, or irritation. Close monitoring by a fertility specialist ensures the correct dosage and reduces the risk of complications during treatment.
4. Human Chorionic Gonadotropin (hCG)
The purpose of these medications is to trigger the final maturation of eggs and induce ovulation at the optimal time. This step is crucial in fertility treatments, as it ensures the eggs are fully developed and ready for retrieval. Commonly used trigger shots include Novarel, Pregnyl, and Ovidrel, which are administered either as subcutaneous or intramuscular injections depending on the specific medication and clinical protocol.
These injections are typically given as a single dose about 36 hours before egg retrieval, carefully timed to maximise the chances of collecting mature eggs. While generally well tolerated, potential side effects can include headaches, irritability, restlessness, and, in rare cases, ovarian hyperstimulation syndrome (OHSS). Careful monitoring and precise timing by the fertility team help reduce risks and ensure the best possible outcome.
Also Read: IVF Side Effects: What You Should ask your Doctor.
5. Progesterone
The purpose of these medications is to support the uterine lining and create an optimal environment for embryo implantation. Progesterone plays a vital role in preparing the endometrium to receive and nurture the embryo, which is why supplementation is a key step in fertility treatments. Commonly prescribed forms include Prometrium, Endometrin, and progesterone in oil, available in different delivery methods such as vaginal suppositories, oral tablets, or intramuscular injections.
These medications are typically started after egg retrieval and continued into the early stages of pregnancy if conception is achieved. While highly beneficial, they can cause side effects such as breast tenderness, bloating, mood changes, and, in the case of intramuscular injections, pain or irritation at the injection site. Despite these possible discomforts, progesterone supplementation is considered essential to support implantation and improve pregnancy outcomes.
6. Estradiol
The purpose of these medications is to thicken the uterine lining, ensuring it is receptive and ready for embryo implantation. By supplementing estrogen, the endometrium can develop to the appropriate thickness, which is crucial for supporting early pregnancy. Commonly prescribed medications for this include Climara and Estrace, which are available in various forms such as oral tablets, patches, or vaginal applications depending on patient needs and treatment protocols.
These estrogen supplements are sometimes used alongside progesterone after egg retrieval, working together to optimise the uterine environment. While generally well tolerated, potential side effects can include nausea, headaches, and breast tenderness. Close monitoring by the fertility team helps to balance hormone levels and minimise any discomfort, ensuring the best possible outcome for embryo implantation. Your doctor will determine exactly how many injections for ivf treatment you’ll need based on your hormone levels and follicle development. On average, patients receive 1-2 injections daily during the stimulation phase, with the total number varying based on individual response to medication.
IVF Process Step by Step: A Comprehensive Timeline
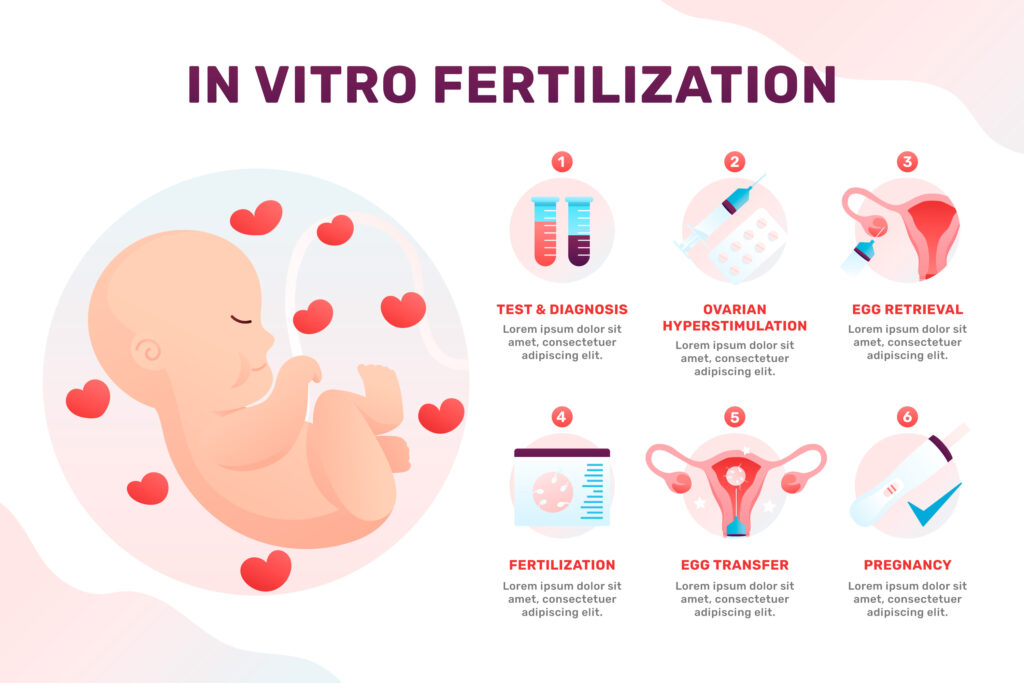
Understanding the ivf process step by step helps patients prepare mentally and physically for each stage of treatment. Here’s a detailed timeline of what to expect:
1. Initial Consultation (1-2 Weeks)
During the initial consultation, patients undergo a comprehensive fertility evaluation that includes a detailed medical history review, hormonal assessments, and an ultrasound. The fertility team also discusses potential treatment options and begins developing a personalised plan. This stage often involves multiple appointments to cover all necessary aspects, including the partner’s semen analysis, baseline blood tests, and further imaging if required. Patients can also expect transparent conversations about treatment costs, potential success rates, and possible risks.

Emotionally, this phase can feel overwhelming due to the amount of information being shared. It’s common to experience mixed feelings of hope and anxiety as the process begins. Asking questions, voicing concerns, and ensuring clarity are crucial steps during this stage to feel more confident and supported in the journey ahead.
2. Pre-Treatment Preparation (2–4 Weeks)
In this stage, patients may be prescribed preliminary medications to prepare the body for stimulation. Fertility specialists often recommend lifestyle modifications, such as dietary changes or exercise adjustments, to support treatment outcomes. In some cases, birth control pills are used to regulate the menstrual cycle before stimulation begins. During this period, patients also receive a final treatment calendar, outlining the timeline and details of the upcoming process.
What to expect includes clear instructions on how to store and administer medications, along with training on self-injections. Monitoring appointments are scheduled, and specific guidance is provided around nutrition, exercise, and daily routines to best support treatment. Emotionally, this stage can bring anticipation and nervousness about starting injections, as well as practical concerns about balancing treatment with daily responsibilities. Many find it helpful to join support groups or seek counselling, offering reassurance and connection during this preparatory phase.
3. Ovarian Stimulation (8–14 Days)
This stage involves daily hormone injections to stimulate the ovaries to produce multiple eggs rather than the usual single egg. Patients undergo regular monitoring with ultrasounds and blood tests to track follicle growth and hormone levels, allowing the fertility team to make medication adjustments based on response. Typically, patients administer 1–2 injections per day, with close guidance to ensure accuracy. Frequent clinic visits every 2–3 days are necessary, and as the ovaries enlarge, it’s common to experience abdominal bloating, heaviness, or discomfort. Strict adherence to the timing of medications is essential to ensure optimal results.
Emotionally, this phase can be challenging. Many patients feel anxious about giving injections correctly, while hormonal fluctuations may trigger mood swings. There is also the stress of waiting to see how the body responds and whether follicles develop as expected. Physical discomfort may impact daily routines, making it important to find ways to rest, reduce stress, and lean on emotional support throughout this intensive phase of treatment.
4. Trigger Shot & Egg Retrieval Preparation (1–2 Days)
At this stage, patients receive the final hCG injection, often called the trigger shot, which stimulates the eggs to complete their maturation process. The timing of this injection is extremely precise, as it ensures that the eggs are ready for retrieval at the right moment. Patients typically undergo one last round of monitoring before the procedure to confirm readiness and fine-tune instructions for retrieval.
During this phase, patients can expect detailed guidance about the exact timing of the trigger shot, along with fasting requirements in preparation for the egg retrieval procedure. It’s also important to arrange transportation and plan for recovery, since sedation is usually used during the retrieval. Emotionally, many feel a mix of excitement at completing the stimulation phase, nervousness about the upcoming procedure, and anticipation about the number and quality of eggs that will be collected.
5. Egg Retrieval (1 Day)
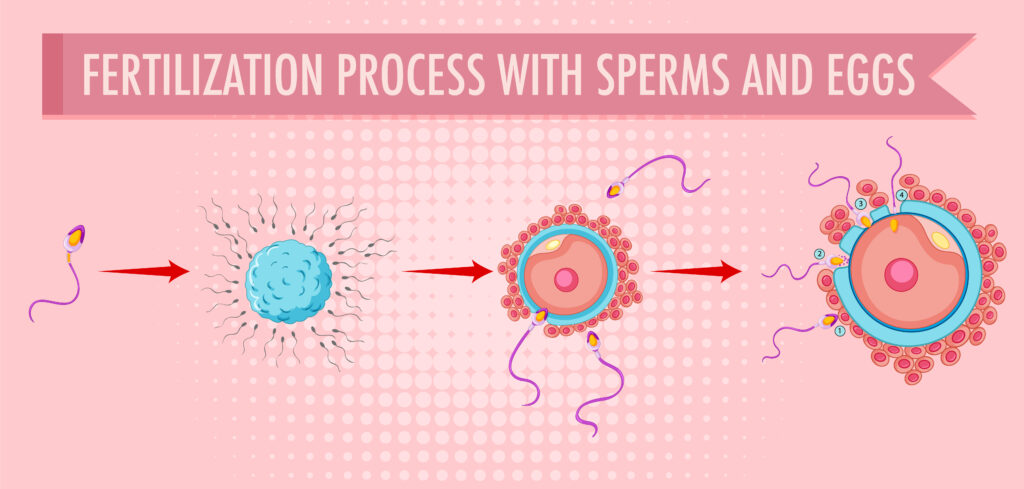
Egg retrieval is a minor surgical procedure performed under sedation, where a transvaginal ultrasound probe with a fine needle is used to collect eggs from the ovaries. Once retrieved, the eggs are sent directly to the laboratory for immediate fertilisation with sperm, marking the next critical step in the IVF process. The procedure itself is relatively short, usually taking 20–30 minutes to complete.
After the retrieval, patients typically spend 1–2 hours in recovery as the sedation wears off. It’s common to experience mild cramping, bloating, or light spotting for a short period afterward. A same-day report on the number of eggs retrieved is usually provided, offering the first indication of the cycle’s outcome. Emotionally, this milestone often brings relief at completing a major stage, but it can also trigger anxiety about fertilisation results and the uncertainty of the next steps. The physical recovery process may add to these emotions, making rest and support especially important during this time.
6. Fertilization & Embryo Culture (3–5 Days)
Once the eggs are retrieved, they are fertilised with sperm in the laboratory using conventional IVF or ICSI (intracytoplasmic sperm injection). Over the next few days, the developing embryos are closely monitored by the embryology team for cell division and growth quality. If chosen, genetic testing (PGT) may also be performed to assess chromosomal health before transfer or freezing.
During this stage, patients can expect daily updates from the lab on embryo progress. Important decisions may need to be made regarding whether to proceed with a fresh transfer or freeze embryos for a later cycle, depending on medical advice and personal preferences. Preparation for embryo transfer continues, with progesterone supplementation playing a key role in supporting the uterine lining. Emotionally, this period can feel intense, with anticipation of daily reports, stress over embryo quality, and sometimes difficult choices when multiple embryos are available.
7. Embryo Transfer (1 Day)
The embryo transfer marks a pivotal moment in the IVF process, where one or more embryos are placed directly into the uterus. This is a quick and generally painless procedure, and patients receive post-transfer care instructions immediately afterward. No anesthesia is required, though a full bladder is often requested to improve ultrasound visibility during the transfer. The procedure typically lasts 15–20 minutes, followed by a brief discussion with the doctor about the number of embryos being transferred.
Emotionally, this stage carries immense significance, as it represents the transition from laboratory work to the possibility of pregnancy. Patients often feel a mixture of hope and caution, with many questions about what activities are safe in the days following transfer. This milestone can be both uplifting and anxiety-inducing, making emotional support and reassurance especially valuable.
8. Two-Week Wait (14 Days)
The two-week wait is the final stage before the pregnancy test, marked by continued hormone support through progesterone injections or supplements. During this time, patients are given specific activity guidelines to help protect the early implantation process and are closely monitored for any complications. A blood pregnancy test is scheduled at the end of this period, with guidance provided on when, if at all, home tests may give reliable results.
Emotionally, this is often described as the most challenging psychological phase of the IVF journey. Patients may experience heightened awareness of every possible pregnancy symptom, leading to hope one moment and worry the next. The anxiety of waiting for the outcome can feel overwhelming, which makes finding healthy distractions, leaning on loved ones, and seeking emotional support especially important during this critical time.
Following the ivf process step by step requires careful timing and monitoring. Your doctor will provide a detailed calendar specific to your treatment protocol, with adjustments made as needed based on your response.
How Many Injections for IVF Treatment? A Complete Breakdown
The question of how many injections for ivf treatment depends on your specific protocol and response to medication. Here’s a general overview:
Typical Injection Schedule
| Treatment Phase | Duration | Average Number of Injections |
|---|---|---|
| Down-regulation (if used) | 7-14 days | 7-14 injections (1 daily) |
| Ovarian Stimulation | 8-12 days | 16-36 injections (2-3 daily) |
| Trigger Shot | 1 day | 1 injection |
| Post-Retrieval/Luteal Support | 10-14 days | 10-14 injections (if using injectable progesterone) |
| Total Range | 26-41 days | 34-65 injections |
The actual number of medications and injections during IVF can vary greatly from person to person. It depends on factors such as your specific treatment protocol (for example, antagonist vs. long protocol), and how your body responds to ovarian stimulation. Some patients may require additional medication adjustments along the way to optimise egg development and reduce risks.
Another factor is the form of luteal phase support prescribed after egg retrieval, which can include progesterone or estrogen in different delivery methods (injections, tablets, or suppositories). Because of these variables, the overall medication plan is highly personalised, ensuring the best chance of a safe and successful outcome.
Managing Injection Discomfort
Many patients worry about the physical and emotional aspects of having to take multiple injections during IVF treatment. While this is a normal concern, there are several practical strategies to make the process more manageable. Simple steps like icing the injection site before administration can help reduce discomfort, while rotating injection sites prevents soreness from building up in one area. Following the proper technique as demonstrated by your healthcare provider is essential for safety and effectiveness, and for injections that are harder to reach, asking your partner or a trusted friend to help can ease the process. Creating a calm, relaxed environment before each injection helps reduce anxiety, and many patients find it helpful to reward themselves afterward to build a more positive association with the routine.
IVF Treatment in India: Costs, Success Rates, and Cultural Considerations
In India, IVF treatment is becoming increasingly accessible, but there are important factors to consider. Costs are generally lower compared to many Western countries, making India an attractive option for patients worldwide, though prices can still vary depending on the clinic, city, and treatment complexity. Success rates are comparable to international standards but depend on factors such as age, fertility history, and the clinic’s expertise. Beyond the medical aspects, cultural considerations also play a role family expectations, societal perceptions, and support systems can deeply influence a patient’s experience of IVF. Understanding these elements, alongside transparent communication with the fertility clinic, ensures patients can make informed decisions while navigating both the physical and emotional journey of IVF.
Many hospitals offering ivf treatment in india now provide package deals that include multiple cycles or money-back guarantees. Some insurance companies have also begun covering certain aspects of fertility treatment, though coverage remains limited compared to other medical procedures.
| Component | Cost Range (INR) |
|---|---|
| Basic IVF Cycle | 1,20,000 - 3,00,000 |
| Medications | 30,000 - 80,000 |
| Additional Tests | 15,000 - 30,000 |
| ICSI (if required) | 25,000 - 50,000 |
| Embryo Freezing | 15,000 - 40,000 |
| PGT/Genetic Testing | 25,000 - 1,00,000 |
Success Rates of IVF in India
The success rates of IVF treatment in India are largely comparable to global standards, especially when performed at accredited and experienced clinics. However, outcomes vary depending on several individual and clinical factors. Age is one of the most significant influences—women under 35 typically have success rates of 40–45%, while this decreases to around 15–20% for women over 40. The cause of infertility also matters, as certain conditions respond more effectively to IVF than others.
Other factors include whether the patient has had previous pregnancies, since this often indicates higher chances of success, as well as the clinic’s expertise and technology, which can significantly impact results. Finally, the type of treatment protocol used plays an important role. Clinics that adopt personalised protocols tailored to the patient’s unique needs tend to achieve better outcomes than those using a one-size-fits-all approach. Overall, while IVF offers hope to many couples in India, individualised care remains the key to maximising success.
Cultural Considerations in IVF Treatment in India
Infertility treatment in India takes place within a unique cultural and social framework, which can deeply influence the patient experience. Family pressure often plays a strong role, as extended families are closely involved in personal decisions and may create added stress around treatment outcomes. Gender expectations also weigh heavily, with women frequently bearing the social burden of infertility regardless of whether the medical cause lies with the male partner, leading to feelings of guilt or isolation.
Privacy concerns are another factor, as many couples choose to keep their treatment private due to social stigma or fear of judgment. At the same time, religious perspectives on assisted reproduction vary across communities and can affect decision-making and acceptance of certain procedures. Traditional family structures in India, while sometimes a source of pressure, can also serve as strong support systems, offering emotional and practical help throughout the IVF journey. Understanding these cultural aspects is crucial for both patients and clinics to create an environment of sensitivity, respect, and reassurance.
Many couples seeking ivf india treatments find support through online and in-person communities. These support networks have become increasingly important in navigating both the medical and social aspects of fertility treatment.
IVF India: Support Systems and Resources for Couples
Professional Support in IVF Treatment
Many IVF clinics in India now recognise the importance of providing comprehensive professional support alongside medical treatment. Fertility counsellors play a key role in helping couples navigate the emotional challenges of infertility, offering coping strategies and a safe space to discuss concerns. Increasingly, clinics are also adopting “phygital” care models, where virtual consultations are combined with in-person treatments, making care more accessible and reducing the stress of frequent clinic visits.
In addition, nutritional support is often provided, with diet plans tailored to improve fertility and overall health during treatment. Some clinics also integrate mind-body programs, including yoga, meditation, and stress-reduction techniques, to enhance emotional well-being and potentially improve treatment outcomes. Together, these professional support services ensure a more holistic approach to IVF, addressing not just the physical aspects of treatment but also the emotional and lifestyle factors that can influence success.
Community Resources
Patients undergoing IVF in India can benefit from a growing network of community-based resources. Online support groups on platforms like WhatsApp, Facebook, and dedicated fertility forums provide safe spaces to share experiences and advice. Patient associations, such as the Indian Society for Assisted Reproduction (ISAR), also offer educational materials and advocacy for individuals and couples. Many clinics encourage peer mentorship programs, connecting newcomers with experienced IVF patients for guidance and reassurance. Additionally, educational seminars—often hosted free of charge—help patients better understand the medical, emotional, and financial aspects of treatment.
Practical Support
Beyond emotional support, there are increasing options for practical assistance. Many cities now have medication delivery services, ensuring patients receive IVF medications conveniently at home. Mobile apps designed for fertility care help with injection reminders, cycle tracking, and appointment scheduling, reducing stress in day-to-day management. Clinics also provide financial counselling, guiding patients through treatment costs, insurance coverage, and payment options. On a broader level, workplace policies are slowly evolving in India, with more employers recognising fertility treatment needs and offering flexibility for appointments and recovery. These resources and services together make the IVF journey more manageable, accessible, and supportive.
Common Questions About IVF Injections and Treatment
FAQ: IVF Injections
Q: Are IVF injections painful?
A: Most IVF injections are administered using thin, short needles that cause minimal discomfort. Many patients report that the anticipation is worse than the actual injection. Techniques like icing the injection site can further reduce discomfort.
Q: Can I administer the injections myself?
A: Yes, most patients learn to self-administer their IVF injections. Your fertility clinic will provide thorough training and often has instructional videos available. Some injections that go into the muscle may be easier with a partner’s help.
Q: What if I miss an injection or give it at the wrong time?
A: Contact your fertility clinic immediately. The importance of timing varies by medication, and your doctor can advise on the best course of action. Never double-dose or skip without medical guidance.
Q: Can I travel during my IVF injection cycle?
A: Limited travel may be possible during certain phases, but you’ll need to coordinate with your clinic. You’ll need to properly store medications, maintain the injection schedule, and ensure you’re back for critical monitoring appointments and procedures.
FAQ: IVF Process and Expectations
Q: How many IVF cycles should I plan for?
A: While some couples succeed on their first attempt, many require multiple cycles. Most doctors recommend planning emotionally and financially for 2-3 cycles for the best chance of success.
Q: What are the signs of ovarian hyperstimulation syndrome (OHSS)?
A: Watch for severe bloating, rapid weight gain, severe abdominal pain, shortness of breath, and decreased urination. These symptoms require immediate medical attention.
Q: Can I work during IVF treatment?
A: Most patients continue working during treatment, though you may need flexibility for appointments. Some take time off around egg retrieval and embryo transfer. Discuss your work demands with your doctor for personalized advice.
Q: How can I improve my chances of IVF success?
A: Maintain a healthy weight, avoid smoking and alcohol, reduce caffeine, manage stress, take prescribed supplements, follow medication instructions precisely, and choose an experienced clinic with good success rates.
Conclusion: Navigating Your IVF Journey in India
The IVF journey involves numerous injections, appointments, and emotional challenges, but understanding each step can make the process more manageable. With India’s growing fertility treatment sector, couples now have access to world-class care with culturally sensitive approaches.
Remember that each person’s experience with IVF is unique. The number and types of injections, timeline, and emotional response will vary based on your specific situation and treatment protocol. Working closely with your fertility specialist and utilizing available support systems can help you navigate this challenging but potentially rewarding journey. If you’re considering IVF treatment, schedule a consultation with a reproductive endocrinologist to discuss your specific situation and determine if this approach is right for
you. With proper preparation and support, you can face the IVF process with greater confidence and clarity.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider for personalized guidance regarding fertility treatments.





