IVF embryo development has helped bring more than 12 million babies into the world through assisted reproductive technologies. High-quality embryos are vital to your chances of successful implantation and pregnancy when you think over fertility treatment.
The trip from fertilisation to transfer has several key stages. These stages span from day 0 to day 5-6 until the embryo reaches the blastocyst stage. Better embryo transfer techniques have led to improved success rates in IVF treatments. The embryo transfer procedure takes just 10-15 minutes. Most patients find it more comfortable than a Pap smear since it needs no incisions or anaesthesia. Doctors now prefer frozen embryo transfers especially when you have the option of genetic testing before implantation. This approach creates better success rates and lowers the risk of genetic defects or miscarriage.
This piece guides you through each stage of embryo development during IVF. You’ll learn about selection criteria, transfer protocols, and what to expect during post-transfer monitoring.
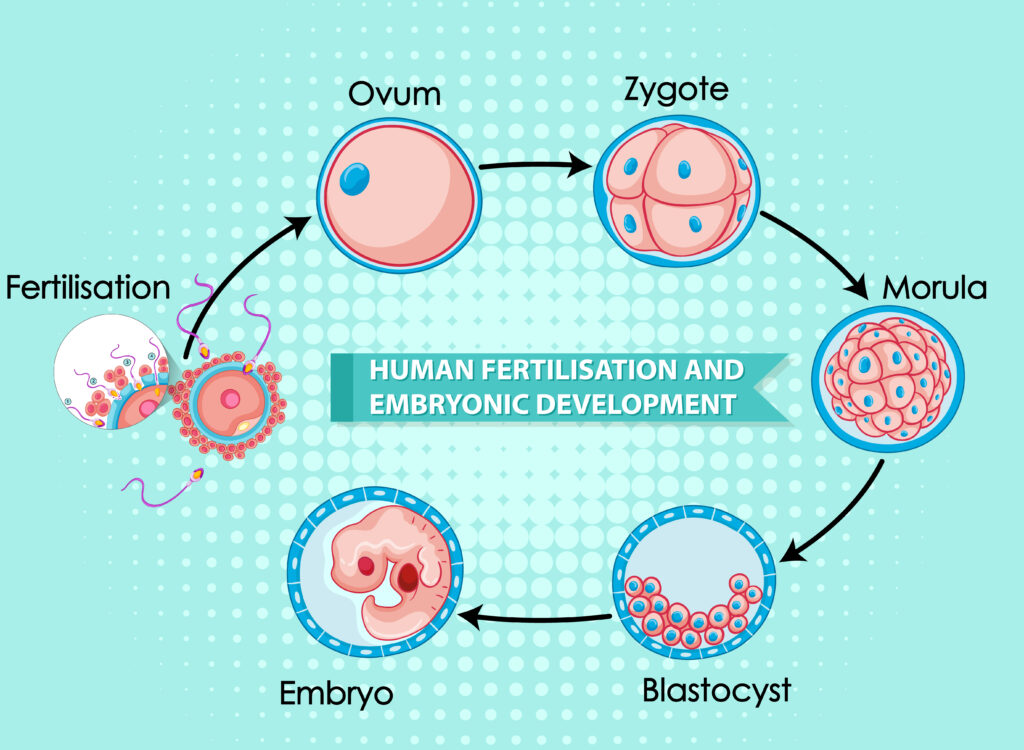
Stages of Embryo Development in IVF
The laboratory experience of an embryo through IVF has several critical developmental milestones that determine its potential to achieve successful implantation and pregnancy.
Day 0: Fertilisation and ICSI vs Conventional IVF
Egg retrieval marks the beginning of the IVF process, followed by fertilisation through conventional IVF or ICSI. Conventional IVF places prepared sperm around eggs in a laboratory dish to allow natural penetration. ICSI takes a different approach by directly injecting a single sperm into each mature egg. Research shows that conventional IVF insemination works best 3-6 hours after egg retrieval, and fertilisation rates reach 84.5% at the time it’s done within 5.5 hours. Doctors recommend ICSI for cases with male factor infertility, though its use now extends beyond the original indications.
Day 1–2: Cleavage Stage and Cell Division
Embryologists check for fertilisation 16-18 hours after insemination. They look for two pronuclei – one has 23 chromosomes from the egg and another has 23 from the sperm. These pronuclei combine in a process called syngamy to form one nucleus with 46 chromosomes. The first cell division happens 30 hours after fertilisation, creating a 2-cell embryo. More divisions follow every 10-12 hours, and by day 2, there’s a 4-cell embryo.
Day 3: Embryo Grading and Assisted Hatching
Embryos typically contain 6-8 cells by day 3. The embryologist’s assessment focuses on cell number, uniformity, and fragmentation. High-quality day 3 embryos have 8 or more cells with less than 20% fragmentation. Doctors might perform assisted hatching at this stage. This procedure creates a small hole in the embryo’s outer shell (zona pellucida) using laser pulses or chemical solutions to help implantation. The procedure usually takes place on day 3 or 4 of development.
Day 5–6: Blastocyst Formation and Trophectoderm Quality
High-quality embryos develop into blastocysts with 100-300 cells by day 5. Scientists grade blastocysts on three criteria: expansion level (1-6 scale), inner cell mass quality (A-C), and trophectoderm quality (A-C). The trophectoderm’s quality is crucial especially when you have to form the placenta. Studies reveal higher live birth rates (55.2%) with early morulation and high-quality trophectoderm compared to 25.5% with late morulation and lower trophectoderm quality. So, letting embryos develop to this stage helps select the most viable candidates for transfer.
Embryo Selection and Grading Criteria
Picking the right embryos plays a crucial role in boosting IVF success rates. Selection methods have evolved from simple morphology checks to cutting-edge genetic testing.
Morphological Grading of Embryos
Embryologists rely on standard grading systems to review embryo quality through visual features. Day 2-3 embryo grading looks at four vital aspects: cell count (4 cells on day 2 and 8 cells on day 3), fragmentation percentage, cell symmetry, and absence of multinucleation. ASEBIR’s A-D grades and Gardner’s numerical system rank among the most accessible grading methods. These systems show that grade A/B embryos with 7-9 cells and less than 20% fragmentation on day 3 have much better chances of implantation. Blastocyst assessment (day 5-6) zeros in on three key parts: expansion level (rated 1-6), inner cell mass quality, and trophectoderm quality (both rated A-C). Research shows that blastocysts with high-quality trophectoderm implant better.
Preimplantation Genetic Testing (PGT-A/PGT-M)
Genetic testing adds more selection criteria beyond morphology. PGT-A checks all chromosomes for numerical abnormalities (aneuploidy), while PGT-M spots specific inherited genetic disorders. PGT-SR serves as another option that finds structural chromosome rearrangements like translocations. PGT-A can increase live birth rates from 25-30% to 52.3% in women aged 38-41 years. It also cuts miscarriage rates from 39% to as low as 2.7% in older patients. The medical community remains split on routine PGT-A use since about 32% of patients might not have any embryos left for transfer after testing.
Choosing Between Day 3 and Day 5 Transfers
Doctors need to think over several factors when timing embryo transfers. Day 5 transfers help pick better embryos since only the strongest ones reach the blastocyst stage. The downside is that some patients might end up with no embryos to transfer if none develop into blastocysts. Day 3 transfers might work better for patients with few embryos or those with poor prognosis. Research shows similar rates of implantation, clinical pregnancy, and live births between day 3 and day 5 transfers. Each patient needs a custom approach based on their embryo quality, quantity, age, and past IVF results.
Embryo Transfer Techniques and Protocols
The last step of IVF treatment involves moving carefully selected embryos to the uterus. This quick procedure affects the overall success rates by a lot.
Frozen vs Fresh Embryo Transfer Protocols
Your specific situation determines the choice between frozen and fresh transfers. Fresh transfers happen 3-5 days after retrieving eggs, while frozen embryo transfers (FET) take place in a later cycle. Research shows frozen transfers work better for high responders (those making 15+ eggs), with higher pregnancy and live birth rates. Patients who produce fewer than six eggs usually get better results with fresh transfers. FET pregnancies also show lower rates of ectopic pregnancy, preterm delivery, and small-for-gestational-age babies.
Ultrasound-Guided Transfer Technique
Ultrasound guidance has become the standard way to do transfers. It’s a great way to get better results. Studies show ultrasound-guided transfers improve clinical pregnancy rates (OR 1.31) and live birth rates (OR 1.47) compared to clinical touch methods. Doctors use ultrasound to see the uterus clearly and place embryos in the perfect spot – about 1-1.5cm from the fundus. This guidance helps even more when transfers are tricky.
Full Bladder Requirement and Catheter Insertion
A moderately full bladder plays two vital roles during transfer. It helps doctors see the catheter better on ultrasound. The full bladder also pushes the uterus down gently, making it easier to guide the catheter through the cervix. Most clinics suggest drinking water before the procedure. Once the catheter is in the right spot, doctors release the embryos and check the catheter carefully to make sure none are left behind.

Post-Transfer Monitoring and Success Factors
The focus changes to supporting implantation and monitoring early pregnancy signs after embryo transfer. This crucial period demands careful management to maximise success rates.
Progesterone Support and Hormonal Monitoring
IVF medications disrupt natural progesterone production, making progesterone supplementation vital after transfer. Doctors recommend continuing progesterone until 8-10 weeks of pregnancy when the placenta takes over production. Patients can receive progesterone through vaginal suppositories, intramuscular injections, or subcutaneous applications. Higher pregnancy rates are linked to progesterone levels >11.83 ng/ml on transfer day during frozen embryo transfers.
Lifestyle Recommendations After Transfer
Patients don’t need strict bed rest but should avoid strenuous activities. A balanced diet rich in leafy greens, protein, and antioxidant-rich fruits helps support implantation. Extreme temperatures might affect the uterine environment, so patients should stay away from hot baths, saunas, or heating pads. Doctors typically recommend avoiding sexual activity for about 15 days after transfer.
Beta-hCG Testing Timeline and Interpretation
Blood tests for Beta-hCG usually happen 9-14 days after transfer. Strong positive results show values above 100 mIU/mL. Early pregnancy levels should double every 48-72 hours. Some clinics test as early as 5 days post-transfer with 93.4% sensitivity using a 4.0 IU/L cut-off.
Factors Affecting Implantation Success
About 32% of euploid embryos fail to implant. Success rates depend on the mother’s age, BMI, endometrial thickness, and embryo quality. Blood presence during transfer procedures reduces success rates substantially (OR 2.35). Lower implantation rates are also connected to chronic endometritis and previous caesarean deliveries.
Conclusion
You’ve now seen how embryo development is a vital part of IVF success. The experience from fertilisation to transfer shows a remarkable process. Skilled embryologists track each developmental milestone with precision. Without doubt, knowing these stages helps you direct your fertility treatment with realistic expectations.
Your embryos go through several key changes. These range from pronuclear formation to cleavage divisions and finally to blastocyst development. Each stage reveals vital details about embryo quality and viability. Modern selection methods like morphological grading and preimplantation genetic testing add extra assessment layers that improve success rates by a lot.
Your specific situation determines the choice between fresh and frozen transfers. Frozen embryo transfers let you do full genetic testing first. Fresh transfers might work better for patients with fewer retrieved eggs. The transfer procedure itself is brief. Yet it needs careful attention to details like ultrasound guidance and proper bladder preparation for the best embryo placement.
Progesterone support becomes vital after transfer to create perfect conditions for implantation. What you do during this waiting period matters too. A balanced diet and right activity levels help your body’s natural processes. Beta-hCG testing gives the first hint of possible pregnancy, usually 9-14 days after transfer.
More than just embryo quality affects success. Your age, BMI, endometrial thickness, and previous reproductive history all affect implantation rates. That’s why personalised treatment forms the life-blood of effective fertility care.
Reproductive medicine keeps moving forward and brings hope to many couples facing infertility. This knowledge enables you to work effectively with your medical team as you think over or move ahead with IVF treatment. You can make better decisions throughout your fertility experience.
Key Takeaways
Understanding embryo development stages helps you make informed decisions during IVF treatment and set realistic expectations for success rates.
- Embryos develop through critical stages from fertilisation to day 5-6 blastocyst formation, with quality assessment at each milestone.
- Blastocyst transfers show higher success rates, but day 3 transfers may be preferable when fewer embryos are available.
- Frozen embryo transfers often achieve better outcomes than fresh transfers, especially for high responders producing 15+ eggs.
- Progesterone support is essential post-transfer, continuing until 8-10 weeks when the placenta takes over hormone production.
- Success depends on multiple factors including embryo quality, maternal age, endometrial thickness, and proper transfer technique
Whilst embryo quality significantly influences IVF outcomes, success rates also depend on individualised treatment protocols, proper hormonal support, and careful monitoring throughout the process. Working closely with your fertility team ensures the best possible approach for your specific circumstances.
FAQs
Q1. What are the key stages of embryo development in IVF? Embryo development in IVF progresses through several stages, starting with fertilisation on Day 0, followed by cleavage and cell division on Days 1-2. By Day 3, embryos typically have 6-8 cells and undergo grading. The blastocyst stage is reached by Days 5-6, with 100-300 cells, which is often considered optimal for transfer.
Q2. When does embryo transfer typically occur in IVF? Embryo transfer in IVF usually occurs either on Day 3 or Day 5 after fertilisation. Day 3 transfers are sometimes preferred when fewer embryos are available, while Day 5 (blastocyst) transfers allow for better embryo selection as only the most viable embryos reach this stage.
Q3. How are embryos selected for transfer in IVF? Embryos are selected based on morphological grading, which assesses factors like cell number, fragmentation, and symmetry. For blastocysts, grading includes expansion level, inner cell mass quality, and trophectoderm quality. Some clinics also use preimplantation genetic testing (PGT) to screen for chromosomal abnormalities or specific genetic disorders.
Q4. What happens after the embryo transfer in IVF? After transfer, progesterone support is crucial to aid implantation. Patients are advised to avoid strenuous activities and maintain a balanced diet. Beta-hCG blood tests are typically conducted 9-14 days post-transfer to check for pregnancy. During this time, the embryo begins to implant in the uterine lining.
Q5. What factors influence the success of embryo implantation in IVF? Several factors affect implantation success, including maternal age, BMI, endometrial thickness, and embryo quality. The transfer technique, including ultrasound guidance and proper catheter placement, also plays a crucial role. Additionally, hormonal support, particularly progesterone supplementation, is essential for creating an optimal environment for implantation.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider for personalised guidance regarding fertility treatments




