Infertility impacts 20% of couples worldwide during their reproductive years, making hormones a crucial element in IVF treatment. Many Indian couples see IVF as a ray of hope, though the complex hormonal processes can seem daunting at first. IVF belongs to a group of assisted reproductive technologies where eggs are fertilised with sperm in a laboratory setting. The treatment’s success depends on maintaining precise hormone levels throughout the cycle. While natural conception typically produces one mature egg monthly, IVF stimulates your ovaries to develop multiple eggs, which improves your chances of pregnancy.
Your body’s hormones play a vital role in fertility and regulate numerous bodily functions. The right hormone balance can make or break an IVF cycle – too much or too little can throw off the entire process. The hormonal changes can also affect your emotional well-being and lead to anxiety, mood swings, and sleep problems.
This piece will help you understand the roles of various hormones in IVF cycles, their monitoring methods, and common challenges Indian couples face. You’ll also learn practical ways to prepare your body for hormone treatment. A better grasp of these elements will help you approach your fertility experience with confidence.

Understanding IVF and the Role of Hormones
IVF stands as a groundbreaking scientific advancement in assisted reproductive technology that brings hope to couples facing infertility challenges. The treatment’s success depends on proper hormonal regulation. Hormones act as biochemical conductors that direct each phase of the IVF process, from egg development to pregnancy establishment.
What is IVF and how hormones support it
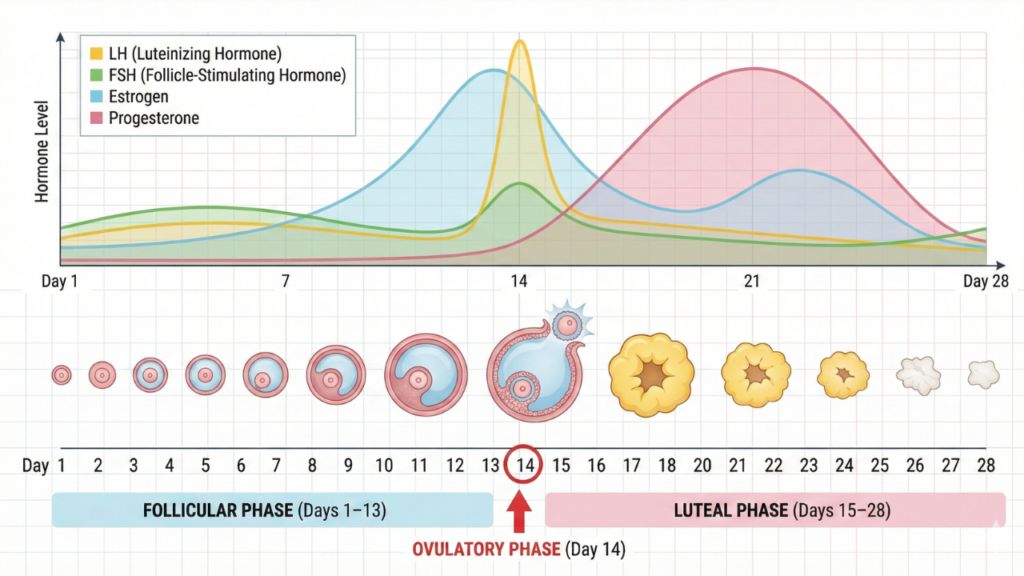
The IVF procedure combines eggs and sperm outside the human body. Medical professionals retrieve eggs from ovaries and combine them with sperm in a laboratory before placing the resulting embryos into the uterus. Hormones play a vital role throughout this process by managing the reproductive cycle. Natural conception usually produces one mature egg monthly. The IVF treatment uses specific hormones to stimulate multiple egg production, which improves pregnancy chances. Doctors administer these hormone medications for approximately eight to fourteen days to ensure proper egg maturation. Hormones and reproduction share an essential connection. FSH and LH work together to boost follicle growth and egg development. The body’s oestrogen builds the uterine lining, while progesterone maintains this environment for embryo implantation. This delicate balance creates perfect conditions for successful fertilisation and pregnancy.
Why hormonal balance is critical for Indian patients
Hormonal balance serves as the life-blood of successful IVF treatment for Indian couples. Any imbalance can affect reproductive outcomes and impact egg quality, embryo implantation, and pregnancy maintenance. The delicate process of conception faces risks from even slight hormonal fluctuations. Indian patients often face unique hormonal challenges. Medical conditions like PCOS, thyroid disorders, and age-related hormonal changes commonly affect Indian women seeking fertility treatments. Dietary habits, lifestyle choices, and stress levels can also throw off hormonal balance. Doctors must create personalised treatment plans for Indian patients based on their individual hormonal profiles and medication responses. Blood tests and ultrasound examinations help doctors adjust hormone dosages to optimise treatment outcomes and reduce side effects.
Overview of hormone stages in the IVF cycle
The IVF cycle features several distinct hormonal stages:
- The first stage focuses on ovarian stimulation using FSH and sometimes LH to encourage multiple follicle development. Some patients take birth control pills or receive injections before treatment to better control their cycle and ensure synchronised egg development.
- Doctors administer hCG as a “trigger shot” once follicles mature to complete egg maturation and prepare for retrieval. Some cases might require leuprolide acetate, a GnRH agonist, to control the stimulation process.
- Oestrogen supplements help thicken the uterine lining after egg collection and fertilisation. Progesterone supplements improve embryo implantation chances and support early pregnancy. Most patients continue these hormones through their first trimester.
- The luteal phase support maintains a uterine environment that helps embryo development. Regular hormone level monitoring ensures optimal conditions for implantation and pregnancy establishment.
- This knowledge about hormonal interventions helps patients better understand their IVF treatment. The process becomes less daunting and more manageable with clear expectations.
Hormones Used in IVF Cycle and Their Functions
The life-blood of successful IVF treatment lies in how well hormones work together. These biochemical messengers create ideal conditions for egg development, fertilisation, and implantation throughout the IVF cycle. Knowing how these hormones work helps you better understand what your body goes through during treatment.
Follicle-Stimulating Hormone (FSH) for egg development
FSH is vital in the early stages of your IVF experience. Your pituitary gland naturally produces this hormone to stimulate follicle growth in the ovaries. Doctors use recombinant FSH (rFSH) during IVF to help multiple follicles develop at once, instead of the single follicle that develops in a natural cycle. The starting dose of rFSH ranges from 100 to 450 IU, with 150 IU working best for average-responders. Patients under 35 usually receive 150 IU daily, while older patients might need higher doses of 225 IU daily. Your doctor monitors your response and adjusts the dose as needed. Too little FSH reduces the number of follicles, while too much can lead to ovarian hyperstimulation syndrome (OHSS).
Luteinizing Hormone (LH) and ovulation control
LH works with FSH to develop follicles and mature oocytes. LH levels during the follicular phase affect the oocyte’s development and its ability to be fertilised. Doctors once thought FSH was enough for successful ovarian response. Research has now showed that LH plays a vital role, especially as follicles reach final maturation. These two hormones need perfect balance, LH changes during the follicular phase can affect the endometrium’s receptivity and pregnancy rates.
Human Chorionic Gonadotropin (hCG) as a trigger shot
The “trigger shot” hCG works like LH to help eggs mature fully and release from the follicle wall. Doctors give this injection when follicles grow to 15-20 millimetres and the endometrial lining reaches at least 7-8 millimetres. Patients get the trigger shot 36-40 hours before egg retrieval. This mimics the natural LH surge that causes ovulation. Patients might feel bloated, have stomach or pelvic pain, or notice tenderness where they got the shot. Patients with high OHSS risk might get Lupron (leuprolide acetate) instead of regular hCG.
Oestrogen for endometrial lining preparation
Oestrogen helps prepare the uterine lining for embryo implantation. Programmed cycles start with oestrogen therapy early in the follicular phase to grow the endometrium while keeping follicles from developing. Patients can take oestrogen as oral tablets, wear patches, or use vaginal rings. Patches keep hormone levels more stable and cause fewer side effects than vaginal methods. Many patients prefer patches because they cause less breast pain (9.1% vs 45.7%) and fatigue (27.3% vs 43.5%).
Progesterone for implantation and early pregnancy
Progesterone gets the endometrium ready for implantation and helps support early pregnancy. Treatment starts on or after egg retrieval day and continues through the first trimester if pregnancy occurs. IVF cycles with progesterone support show much better pregnancy rates than those without it. Patients can receive progesterone through muscle injections, vaginal suppositories, gels, or tablets. Oral progesterone doesn’t work well enough to support pregnancy. Most Indian patients use vaginal progesterone because it works as well as injections without causing injection-site pain.
GnRH Agonists and Antagonists for cycle regulation
GnRH agonists and antagonists stop early LH surges during ovarian stimulation. GnRH agonists first boost FSH and LH release but then suppress them when used continuously. This works well but might cause hot flushes and headaches. GnRH antagonists suppress gonadotropins right away without the initial boost, which means shorter treatment time. These protocols also lower OHSS risk, making them more popular. Indian patients with high OHSS risk often do better with antagonist protocols using GnRH agonist triggers, which can eliminate this serious complication.
Monitoring Hormone Levels During IVF Treatment
Your IVF cycle needs regular monitoring to keep hormone levels balanced. This helps doctors make vital adjustments that can improve your treatment results by a lot. Indian couples going through fertility treatment need this personalised care to succeed.

Blood tests for FSH, LH, oestrogen, and progesterone
Blood hormone testing starts on day 2 or 3 of your menstrual cycle. This gives doctors your baseline levels before stimulation begins. Your doctor will check key hormones like oestradiol (oestrogen) and progesterone regularly during the stimulation phase. Oestradiol levels associate directly with how big and numerous your follicles are. These levels often match what ultrasound scans show.
Your oestradiol rises as follicles grow, so doctors can tell how well your ovaries respond to medication. Progesterone tests serve two vital purposes. High progesterone before egg collection might mean freezing all embryos instead of doing a fresh transfer. After embryo transfer, doctors keep checking progesterone to spot any absorption issues that could affect implantation. Indian patients with PCOS or thyroid disorders need these hormone tests. The results show how your body responds to treatment and let doctors adjust medications precisely.
Ultrasound tracking of follicle growth and uterine lining
Transvaginal ultrasound scans are the life-blood of IVF monitoring, along with blood tests. You’ll typically have 3-5 ultrasound examinations during ovarian stimulation. Each scan carefully measures your follicle count, size, and endometrial thickness. Doctors track your follicle growth until they reach the right size. They look for 2-3 main follicles larger than 17mm. Women over 39 or those who responded poorly before might need follicles to reach 20mm before triggering. The ultrasound also checks your endometrial thickness (EMT). Your uterine lining needs proper preparation for implantation. This detailed approach helps fertility specialists see how you respond to hormone medications.
Adjusting hormone doses based on patient response
Your treatment plan changes based on how you respond to hormones. The original FSH dose (usually 150-225 IU daily) might change after 3-5 days. Doctors can adjust it by 75-150 IU, but won’t go over 450 IU/day. Indian patients with unexpectedly low response might need more FSH to get more eggs. Those who respond too strongly might need less medication to avoid ovarian hyperstimulation syndrome. This careful monitoring lets doctors make vital adjustments. You’ll get better results with fewer side effects. Your fertility specialist will fine-tune your treatment based on your unique hormone levels and how your ovaries respond.
Common Hormonal Challenges Faced by Indian Couples
Many Indian couples encounter hormonal complications during IVF treatment despite careful monitoring. A better understanding of these challenges will help you direct your fertility experience with confidence.
Ovarian Hyperstimulation Syndrome (OHSS)
OHSS develops when ovaries overreact to stimulation medications and leak fluid into the abdomen. Mild OHSS affects approximately 33% of women undergoing IVF, but only 1% develop moderate or severe forms. Indian women with PCOS face a higher risk. The symptoms can range from mild abdominal discomfort to severe complications. These include fluid collection, kidney problems, and in rare cases, blood clots.
Low ovarian response and poor egg yield
Low ovarian response creates a major obstacle and affects 9-24% of patients undergoing IVF. Patients produce fewer than 3-5 follicles despite hormone stimulation. The risk is highest for Indian patients over 40, who make up 76% of poor responders. Live birth rates stay low at 2.3% to 8.7% per started cycle, even with the best stimulation protocols.
Hormonal imbalances due to PCOS or thyroid issues
PCOS remains the most common endocrine disorder in Indian women of reproductive age. The condition often occurs alongside thyroid dysfunction, which creates complex hormonal challenges. Research shows that PCOS patients have a 2.5 times higher risk of thyroid disease. Women with PCOS face an elevated risk of subclinical hypothyroidism compared to those without the condition.
Emotional and physical side effects of hormone injections
Hormone medications can cause headaches, hot flashes, and bloating. Women often notice soreness, redness, or mild bruising at injection sites. The hormonal fluctuations lead to mood swings, anxiety, and sleep disturbances. These emotional effects create additional stress for Indian couples who are already dealing with fertility treatment challenges.
Also Read: How to Improve IVF Success: Essential Diet and Lifestyle Changes
Preparing for Hormonal Treatment in IVF
The right body preparation for hormonal medications can boost your IVF success rates. Your lifestyle choices create the perfect environment for hormones to work well during your fertility treatment.

Lifestyle changes to support hormone balance
Regular physical activity plays a vital role in hormone regulation. Simple exercises like walking, swimming, or yoga help blood flow to reproductive organs and improve hormone function. However, too much high-intensity exercise might harm fertility and throw hormones off balance. You’ll get the best results with gentle exercises that don’t strain your abdomen.
Sleep is the life-blood of hormonal health. Your body needs 7-8 hours of sleep each night to regulate reproductive hormones. Research shows that melatonin, which regulates both sleep and reproduction, reaches its peak between 9 p.m. and midnight. This makes 10-11 p.m. your ideal bedtime. Your reproductive health improves when you stay away from endocrine-disrupting chemicals in certain plastics and household products. These substances can mess with normal hormone function and affect your fertility.
Dietary tips for better hormonal response
A Mediterranean-style diet shows great promise for IVF success, especially when you have women under 35. This diet focuses on fresh fruits, vegetables, lean proteins, whole grains, and healthy fats. Foods rich in antioxidants—like berries, nuts, and leafy greens—protect your reproductive cells from damage. High-protein foods such as eggs, legumes, tofu, and lean meats help with optimal egg production. Foods with omega-3 fatty acids, including flaxseeds, walnuts, and salmon, reduce inflammation that might disrupt hormone balance. Good hydration supports your uterine health and helps your body absorb nutrients. Water or coconut water can prevent bloating and support natural detoxification.
Importance of stress management and emotional support
IVF treatment creates emotional strain that matches the stress of losing a family member. Research proves that stress won’t stop conception or reduce IVF success rates, but managing it helps your overall wellbeing. Mind-body techniques help control stress hormones. Meditation, deep breathing exercises, and gentle yoga reduce anxiety levels. Reading and journaling give you emotional outlets during this challenging time. Professional counselling provides a safe space to explore your fertility-related emotions. Therapists who specialise in fertility issues offer practical coping strategies and unbiased guidance. Support groups, both in-person and online, help you connect with others facing similar challenges and reduce isolation.
Working with a fertility specialist for personalised plans
Success in fertility treatment comes from personalised care. Each couple’s treatment needs are different, which calls for individual attention to maximise success rates. Your fertility specialist should review your medical history, diagnostic tests, and previous treatments to create your custom plan. A detailed approach looks at your medical needs, lifestyle factors, emotional wellbeing, and priorities. This includes custom medication protocols, nutrition advice, and psychological support services. Regular check-ups let your doctor adjust treatment based on your response. This ongoing personalisation improves your success chances while reducing physical, emotional, and financial stress.
Conclusion
The complex world of IVF hormones might seem daunting at first. In spite of that, knowing how these chemical messengers work throughout your fertility experience enables you to take a more active role in your treatment. Your body’s response to these carefully adjusted hormones ended up determining the success of each IVF cycle. Many Indian couples face specific hormonal challenges that need extra care. PCOS and thyroid disorders are especially common among Indian women and need personalised hormonal protocols. Close collaboration with specialists who understand these unique needs is vital to achieve the best results.
Your fertility team uses blood tests and ultrasound scans to monitor hormone levels and make vital adjustments to your medication. This personalised approach improves your success chances by a lot while lowering the risk of complications like ovarian hyperstimulation syndrome. Without doubt, lifestyle choices play a vital role in maintaining hormonal balance throughout your IVF experience. Your body responds better to treatment with a balanced Mediterranean-style diet rich in antioxidants, moderate exercise, and good stress management techniques. Small adjustments like these can make a real difference in treatment outcomes.
Emotional health needs equal focus during hormonal treatment. Hormone medications can affect your moods on top of the stress from fertility treatment. Support groups for Indian couples going through IVF are a great way to get emotional support during this challenging time. IVF is a big commitment, physically, emotionally, and financially. Challenges may come up along the way, but knowing each hormone’s purpose and effects helps make the process clearer. Your determination combined with medical expertise gives you the best chance to meet your dream of parenthood.
Key Takeaways
Understanding hormones in IVF empowers Indian couples to navigate fertility treatment with greater confidence and realistic expectations about the complex process ahead.
- IVF success relies on precise hormonal balance – FSH stimulates multiple egg development, whilst hCG triggers final maturation and progesterone supports implantation
- Regular monitoring through blood tests and ultrasounds allows doctors to adjust hormone doses, optimising outcomes whilst minimising risks like OHSS
- Indian women face unique challenges including higher PCOS rates and thyroid disorders, requiring personalised hormonal protocols from experienced specialists
- Mediterranean-style diet, moderate exercise, quality sleep, and stress management create optimal conditions for hormones to function effectively during treatment
- Professional counselling and support groups help manage emotional side effects of hormone fluctuations, which can significantly impact wellbeing throughout the IVF journey
The intricate dance of hormones throughout your IVF cycle may seem daunting, but each medication serves a specific purpose in creating the best possible environment for conception. By understanding these processes and preparing your body through lifestyle modifications, you’re taking active steps towards achieving your dream of parenthood.
FAQs
Q1. What are the key hormones used in IVF treatment? The main hormones used in IVF include follicle-stimulating hormone (FSH) for egg development, luteinizing hormone (LH) for ovulation control, human chorionic gonadotropin (hCG) as a trigger shot, oestrogen for endometrial lining preparation, and progesterone for implantation support.
Q2. How are hormone levels monitored during IVF? Hormone levels are monitored through regular blood tests and ultrasound scans. Blood tests measure FSH, LH, oestrogen, and progesterone levels, while ultrasounds track follicle growth and uterine lining thickness. This allows doctors to adjust hormone doses based on individual patient responses.
Q3. What are common hormonal challenges faced by Indian couples during IVF? Indian couples often face challenges such as ovarian hyperstimulation syndrome (OHSS), low ovarian response, and hormonal imbalances due to conditions like polycystic ovary syndrome (PCOS) or thyroid issues. These can affect treatment outcomes and require careful management.
Q4. How can couples prepare for hormonal treatment in IVF? Couples can prepare by making lifestyle changes to support hormone balance, such as maintaining a healthy diet rich in antioxidants, engaging in moderate exercise, and managing stress through techniques like meditation or yoga. Working closely with a fertility specialist for a personalised treatment plan is also crucial.
Q5. What are the potential side effects of hormone injections during IVF? Hormone injections can cause both physical and emotional side effects. Physical symptoms may include bloating, headaches, and injection site soreness. Emotional effects can include mood swings, anxiety, and sleep disturbances. It’s important for couples to be aware of these potential effects and seek support when needed.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider for personalised guidance regarding fertility treatments





